2023 Caregiver Survey
Our survey of more than 100 unpaid family caregivers provided us with valuable insights.
2023 Caregiver Survey
Our survey of more than 100 unpaid family caregivers provided us with valuable insights.
Our innovations are grounded in actual data obtained from real caregivers.
Understanding Caregiver Experience
This survey interviewed 119 American unpaid caregivers about their overall caregiving experiences, struggles, and complications. There was a relatively equal sample of male and female participants, with 65 (54%) females, with the remaining 54 (46%) identifying as male. 7 (.05%) Participants identified as Asian, 14 (11%) as Black, and 90 (75%) as White. The remaining (14%) participants were of mixed race. The average age of participants was 45 years old. 62 (52%) participants had a full-time job outside of caregiving, 15 (12%) worked part-time, 8 (.06%) were unemployed and searching for a job, and the remaining participants were unemployed and not job-seeking (this category includes homemaking, full-time unpaid caregivers, and retirees under the same umbrella).
To begin, the survey prompted caregivers to describe their caregiving experience, as well as answer questions related to what would benefit them as a caregiver.
60% of the caregivers had been providing care for 1-5 years, while 28% had provided care for more than five years. Only one participant was relatively new to providing care with less than a year of experience. Additionally, 53% of caregivers surveyed were caring for only one loved one, while 37% were caring for 2-3 friends or family. Only 9 participants provided care for more than three people.
Caregivers spent a variety of time caregiving for their loved ones, with the majority (40%) spending 10-20 hours per week providing care.
The average rating for the difficulty of their role as a caregiver was 3 out of 5 (a moderate level of difficulty). Additionally, the average difficulty rating for organizing and consolidating data was 2 out of 5 (a low-moderate level of difficulty).
Caregivers were then asked to rank the importance of organizational tools, community and encouragement, and having a place to get answers for their caregiver needs.
This data had a wide range of results. Most caregivers surveyed were generally positive about having access to organizational tools, community, and a central place to get answers. The rankings in order of importance were having a place to get answers (most important), organizational tools (second importance), and the least important for the surveyed caregivers was access to community and encouragement.
Next, the greatest struggle (or information they wish they had known) for caregivers beginning their caregiving journey was overwhelmingly learning how to balance their professional and personal lives (48% reported this was the most important piece of information they needed to know). The second most important was financial knowledge, followed by skills to care for an aging parent.
The least important (as far as the education they had wanted at the beginning) was learning medical knowledge.
Caregivers were asked about what technologies they used for their caregiving endeavors. Respondents used a variety of tools including apps such as ianacare, devices such as grandpads, Amazon Alexa devices, cellphones, medical alert bracelets, in-house alarms/doorbell systems, in-home support such as maids or aids, as well as meal delivery systems like Hello Fresh, Instacart, or store delivery.
84% of participants agreed that having an application where information and tools were consolidated would benefit their overall caregiving experience, and 61% were willing to pay for an application or in-person support.
When asked about what types of support they would be willing to pay for or benefit from, 33% said in-home care would be the most beneficial, followed by an administrative aide (30% of respondents). The services participants were least likely to pay for were both tied between a caregiver support application and a 24/7 care support hotline (19% of participants would be willing to pay for these features). Additionally, when asked if they would be willing to pay for a caregiving application, participants had mixed responses: 30% were unwilling to pay any amount of money for an application, 39% were willing to pay no more than $10, and finally, 9% were willing to pay $20 or more.
Additionally, when asked how they preferred to pay for an application (weekly, monthly, or yearly), 5% of participants were in favor of a weekly subscription model. 76% of participants were in favor of a monthly subscription, with the remaining 19% responding favorably to an annual subscription model.
Next, the most important services or activities for general well-being were ranked as: sleep (58% of respondents ranked this as completely necessary), and an understanding employer (41% marked as completely necessary). Other notable responses included 56% of caregivers surveyed noting that extra help around the home, exercise (41%) employer health benefits, and an all-in-one tool (38%) would be very important. Finally, participants were generally (28%) neutral about speaking with a therapist and being paid to be a caregiver as it pertained to their overall well-being.
57% of respondents noted that having a support team would make their caregiving somewhat easier.
When asked about what areas of coordinating support with their family they needed help with, 40% of respondents noted that they needed assistance with household chores and social time. Notably, 46% of respondents said that staying on top of the text and email threads was not an area they needed any assistance with at all. Additionally, 58% said Medicare and insurance were where they required the most professional assistance, followed by care and end-of-life expenses (50%). The area they required the least professional assistance was taxes (14%).
Health-Related Responses
Caregivers were then asked questions related to health and well-being, both for themselves and their care receiver.
When asked about changes to their health and medical needs, respondents were split in their health changes. 54% of participants did not require increased medical care since becoming a caregiver, while 27% experienced an increase in emergency, telehealth, primary care, or specialized doctor visits since becoming a caregiver. Additionally, 24% started therapy or sought mental health support, and 15% had started new medications. 61% of participants reported a decline in mental health after beginning caregiving, with an additional 32% noting a decline in health as well.
Concerning their care receiver’s health, 46% of participants reported that they took their loved one to regular (planned, necessary, or otherwise anticipated) doctor’s appointments one to three times per month. 36% reported quarterly visits, while 10% brought their loved ones to doctor’s appointments weekly. When asked about preventable emergency department visits, 35% of respondents had one or two preventable ER visits annually, although participants noted that these visits were due to slip/fall accidents and were mobility related, and generally unpreventable in the sense that falls would happen regardless of safety measures. Additionally, 45% of participants reported no unnecessary ER visits. Next, 49% of respondents reported taking their loved one to an unplanned (but non-emergency) doctor’s visit about once every six months.
With regard to health and well-being, as it relates to nutrition, 67% of interviewed caregivers shopped for groceries in person at a store. 22% ordered groceries for delivery/pickup, and only 3% of participants routinely used meal delivery kits such as Hello Fresh or Blue Apron.
App Related Responses
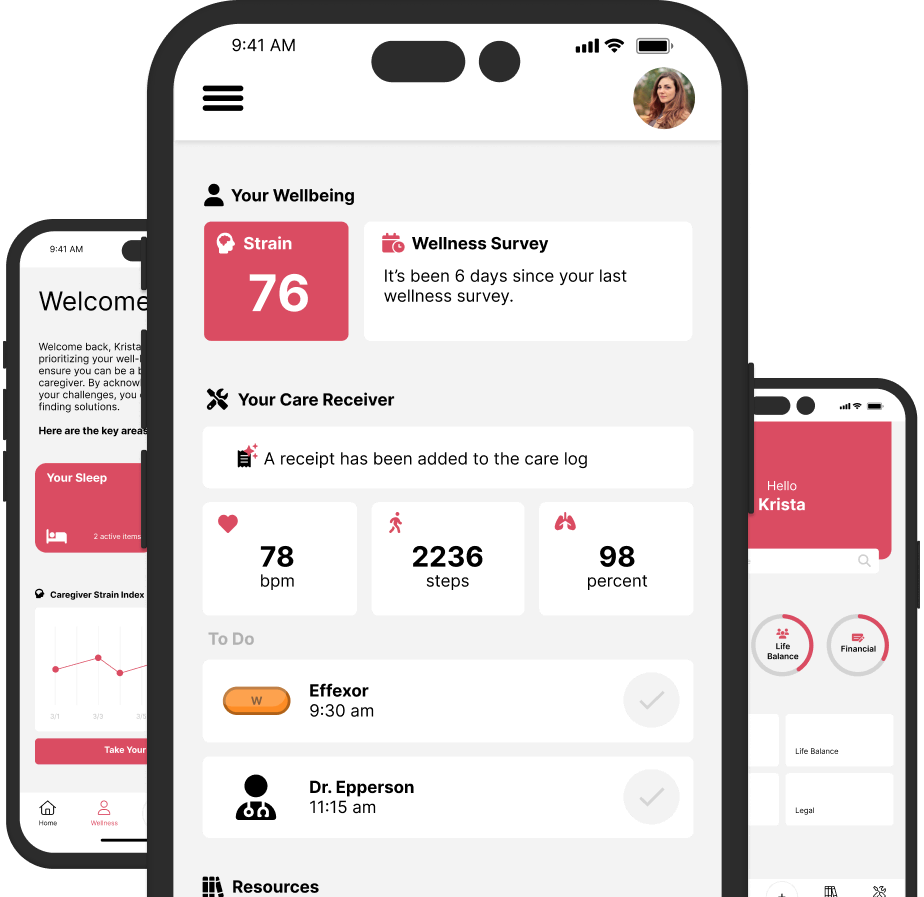
The next questions asked of participants related specifically to what features (or functionality) they would use (or find beneficial) in a mobile caregiving application.
The ability to have in-app permissions was split between participants, with 64% in support of having permission settings for their appointed care team.
When asked what tools would be useful in a caregiving application, 65% reported that having tools to help them track medications, schedule appointments, and shop for groceries for their loved ones was the most important.
With regard to care receiver-oriented app features, participants were generally neutral about what they would use. 28% of participants responded that having a way to keep their appointed support teams up to date with information related to their health and well-being (specifically stress and workload) would be something they used all of the time. 25% of participants noted that resources to manage and balance relationships (marriage, children, kids, the care receiver) would be used all of the time, with the remaining responses (30%) being neutral (would neither find useful nor useless) about the functionality of features such as a diet log, hydration goals, calming features, and health and exercise goals. Ultimately, features specifically relating to the caregiver were not reported as being important.
Next, the ability to keep their appointed teams up to date and informed was rated as being neutrally important, with the average response being a 3 out of 5 for importance. 90% noted that having a team of informed friends and family equipped with insights into their stress loads would help them be well-balanced, supported, and mentally healthy caregivers. The ability to use a self-analysis feature to stay self-aware about individual stress and inform their appointed care support teams was also consistently ranked as a 3 out of 5 for importance, suggesting users would generally appreciate a holistic team-based approach to their caregiving systems.
In this regard, having the ability to share the workload with their support team in an app was reported by 30% of participants as being something they would use all of the time, followed by an easy way to notify the support team of information.
When answering questions regarding how they would use a caregiving app, 40% of the surveyed caregivers reported that resources to manage their relationships while caregiving would be used frequently. 53% noted that having simple exercise and health goals would be something they used occasionally, followed by (40% for each respectively) diet logs and meditation/relaxation features.
Participants also answered questions about the most important features an application could offer them.
Based on participant responses, the top three most useful app features for caregivers are tools to help them track medications, schedule appointments, and shop for groceries for their loved ones was the most important (65%), followed by automating and storing medical records (58%), and appointment tracking/calendar synchronization (57%).
With regard to other additional app features, automatic health & doctor record updates (46% said they would use a feature like this), fall detection (42%), and appointment/schedule tracking (35%) were noted as being the most potentially useful features.
Qualitative Analysis
Caregivers were asked to provide short answer responses to questions about their overall experiences in caregiving. These responses were analyzed for themes described below.
Common Challenges
Caregivers were first asked to describe some of their caregiving experiences and challenges. Common themes for challenges across responses were time, exhaustion, nutrition, and financial struggles.
Time
The first common theme was time. Having enough time, having personal time, balancing it all, and managing stress were common responses surrounding caregiving challenges. One participant noted that their biggest challenge was
“Balancing my work, caregiving time, and time for myself. Sometimes I feel like I don't have time to take care of myself because I'm taking care of my disabled mom and my son and working a full-time job as well as cleaning the house and taking care of the yard work. It sometimes feels like a never-ending cycle of things I have to do and little time to rest and focus on myself.”
Additionally, having enough time, juggling multiple tasks, and making time for self-care was common pain point among the surveyed caregivers. Balancing self-care and caregiving was a balance that is important for caregivers to strike:
“making sure that needs are met on both sides. Not just for the person I am caring for, but my own needs as well, I don't want to shortchange them or myself so it kind of can become a balancing act, but not too much as it is not a full-time thing. Some days time is a little more pressed than others, but that is usually the number one thing I run into.”
Exhaustion.
Similarly to having enough time, caregivers reported exhaustion as a challenging aspect of their caregiving journeys. For instance, caregivers noted that
- “my fatigue is a difficult part of the process, but being tired and not knowing what to expect from the person I'm taking care of is the most difficult part of the process” and that
- “being constantly tired and worn out and dealing with the anxiety associated with worrying about the people I am taking care of” was the most pressing challenge in their caregiving experience.
- Anxiety surrounding exhaustion was another concern: “being constantly tired and worn out and dealing with the anxiety associated with worrying about the people I am taking care of”, and “being fatigued and tired and never really having a true day off” were common challenges.
Financial Struggles.
Having enough money and navigating the financial costs of caregiving was another challenge for caregivers. Caregiving takes away from the participants’ time “to make an income”, making it difficult to “balance work [and earn an income]” and adds complications to the delicate balance of professional work and caregiving work. “The financial responsibility and equally being in charge of making difficult decisions for another human being” and “with work, I find it hard to find the time to devote to caring for my father-in-law and his needs continue to increase.”
Nutrition.
Providing adequate meals, knowing what to cook, picky eating, and finances were all common themes associated with the challenges of providing nutrition for care receivers.
For instance,
“One of the people I care for has an extremely specialized and restrictive medical diet. Keeping things interesting and tasting good can be very hard to keep up with. It requires a lot of time in the kitchen. They are not the only person I can for [I have a family to care for as well], so keeping up with several diets in one place is extremely hard. Also, the cost of the specialized food items is extremely high.”
Dietary restrictions are often combined with more expensive ingredients, which can both impact the caregivers' finances as well as their time. Providing loved ones with food that was nutritious and appropriate for their diets as well as something they would eat proved to be challenging as well:
“She somewhat eats like a child. She has wanted to stay the same and are almost always the things she doesn't need or actively make the situation worse. Sweets, carbs, etc. The only difficulty I could express is being able to get her to eat healthier, having to pick between giving her what she wants to eat and her becoming upset that I'm withholding the food she wants”
“they often refuse to eat anything healthy, or they refuse to eat in general. Sometimes, the only things they want to eat are quite expensive.”
Nutritious foods often proved to be more expensive, and caregivers reported financial strain as a result:
“rising grocery prices making shopping on a budget more difficult”, and “prices are unreal”.
Finally, caregivers reported that picky eating was a common struggle they experienced with their loved ones’ nutrition.
“I cook and buy nutritious meals, but she likes peanut butter cups”,
“The person for whom I'm caregiving needs to follow a low-sodium, heart-healthy diet due to cardiac issues, so it can be difficult making meals that follow these guidelines from scratch that are still something they would like to eat”, and
“They seem to want the foods that are not the best as they are their favorites. Sometimes they seem not to care about how unhealthy they are while needing to be on a certain diet. You want to accommodate them knowing they perhaps have more time behind them but you want also want to make sure they are enjoying their lives presently.” Managing Stress The respondents were then asked about what would help them manage their stress as a caregiver. Common themes among responses were financial support, relational and emotional support, and task support. Financial Support. Finances were a common stressor for caregivers. One participant noted that “the most stress for me is the financial part. I don't know what could help me manage that”, another noted “having more money” would relieve some of their caregiving burdens, and another commented that having support services covered by insurance would bring some relief. When acting as an unpaid caregiver, finances and the cost of caregiving were of great stress to participants. Ultimately, finding ways to ease the financial burden would help the surveyed caregivers manage their stress more effectively. Relational and Emotional Support. Balancing it all was another common stressor for caregivers. “I think something that would help me manage my stress as a caregiver is just having someone who cared as much as I do about the person. When you are the only one worried about things, and the only one who does anything it makes the worry and work that much more difficult. Having someone else who is there and cares, and can take over sometimes would be very nice.” Uniquely, balancing it all without being a burden on their loved ones was a great point of stress. “More help from family members would be great”, and “a helping hand and probably someone to talk to who is dealing with the same thing and being able to give me hands-on tips on how to deal with certain things that may arise” was noted as being helpful. Caregivers also wanted support, but it was complicated: “I am not sure what I could use to help manage stress for myself but it sure would help me a great deal. I don't want my friends and family to see my stress and take it personally. That would break my heart” suggesting that oftentimes the stress itself was a source of stress. Caregivers did not want to add additional worry to their family's plates and would hide the challenges they experience with being an unpaid caregiver to spare their loved ones further concerns. For example: “having a central person who would be like a liaison who could point me in the right direction as to who to ask about services that my parent(s) need. Sometimes I have to call around to quite a few places before I find out answers about insurance or specialty doctors or financial assistance, etc. If there was a central place to find that out, that would be very helpful” And, “I am the only other family member locally, so me and my family bear the burden of caring for my mother. My sibling contributes financially but lives across country so I and my partner have to sacrifice our time for the caregiving. My mother is declining so the intensity of her care is increasing as well and there just aren't a lot of resources locally for family caregivers.” Consequently, caregivers would often take their care into their own hands rather than ask for outside support. “I learned the hard way that I needed to take care of myself first. I got burned out during the first 9 months because I wasn't looking out for myself. I wish I had someone who was looking out for me and warning me to take care of myself.” Task Support. As mentioned before, caregivers were often stressed about managing it all, and one noted “I would find it useful if my sister would step up and help more with my mom, or my son would help out more with things that need to be done around the house” while another noted that having “someone to share duties with” would help their overall stress. Having general support without asking for it would be beneficial for the respondents, and communicating needs without having to ask for help would aid in the caregiver experience: “I would like the family to spend more time with the help” and “having other people know schedules and important information” were generally important to caregivers. Notably, “knowing that time may seem jam-packed with tasks or chores but that it’s important to have time to relax with the loved one and not only interact when doing actual care tasks.” So, while caregivers did not want to add a burden to their loved ones' lives, they also hoped their support teams would notice that there were tasks that needed accomplishing without them having to ask for help. Managing Information Finally, caregivers were asked questions regarding the challenges associated with keeping their family involved in managing their care receiver’s information. Common pain points included managing medication and appointment information, and, communication and coordinating with family. Managing medication and appointment information. Managing tasks and information was a frequent theme across all responses to questions. One caregiver noted that “juggling multiple appointments or medication schedules with my responsibilities in caring for my own children and their school transportation as well as my own appointments is a challenge but a shared schedule or calendar can help with this” and support teams lacking the education to support care receivers : “being able to delegate time and explain different medical terms” were also reported as pain points: “Sometimes they cannot remember what they have and have not done so i have to spend time trying to figure it out which can be challenging when you are not the patient.” Finally, tracking medication and relaying what happened at doctor appointments were also areas of struggle across family teams. Communication and Coordinating with family. Communication and coordination with family was major pain point for caregivers, from managing schedules to sharing information. For instance, “sometimes communication gets a bit staticky. And then everything seems to fall apart regarding being organized and all on the same page. People then get cranky and that's when I need a bit of help”, and “I have a large extended family. so it can be hard to keep everyone in the loop in regards to giving them information about how our loved one is doing and what upcoming appointments we have and what our schedule looks like from week to week”. Family disengagement was also a common issue: “other family is far away and not very in tune with actual caregiving needs”, “they all live far away and pretend they don’t see my texts”. Similarly, “it is challenging to keep my family involved. I am the only sibling living close to my parent. I have one sibling who lives out of state and the other one lives about one hour away. I try to keep them informed by calling or texting.” Coordinating care and information without feeling like a burden, having family step up to the plate for support tasks, and navigating information sharing with family across the country proved to be difficult for caregivers. “My husband and I are the only responsible family members for my father and his mother within our state so it is impossible for other family to help out. If they need something, we are the only ones available, but we don't have the financial resources to pay for any services or pay for extra help.” Finally, “my family doesn't live nearby so an app that I could update daily would be amazing so they can log in, see how she's doing daily, and maybe even face time with her would be awesome. It is so hard to complete daily tasks around the house, as well as upkeep the caregiving and work a full-time job just to afford all of this.”